- If the anterior is elevated treat it as abnormal
- If there is a posterior fat pad at all, treat as abnormal as 75% have fractures.
2. Anterior humeral line
On the lateral, draw a line down the anterior surface of the humerus. 1/3 of the capitellum should lie above the line.
3. Radiocapitellar line
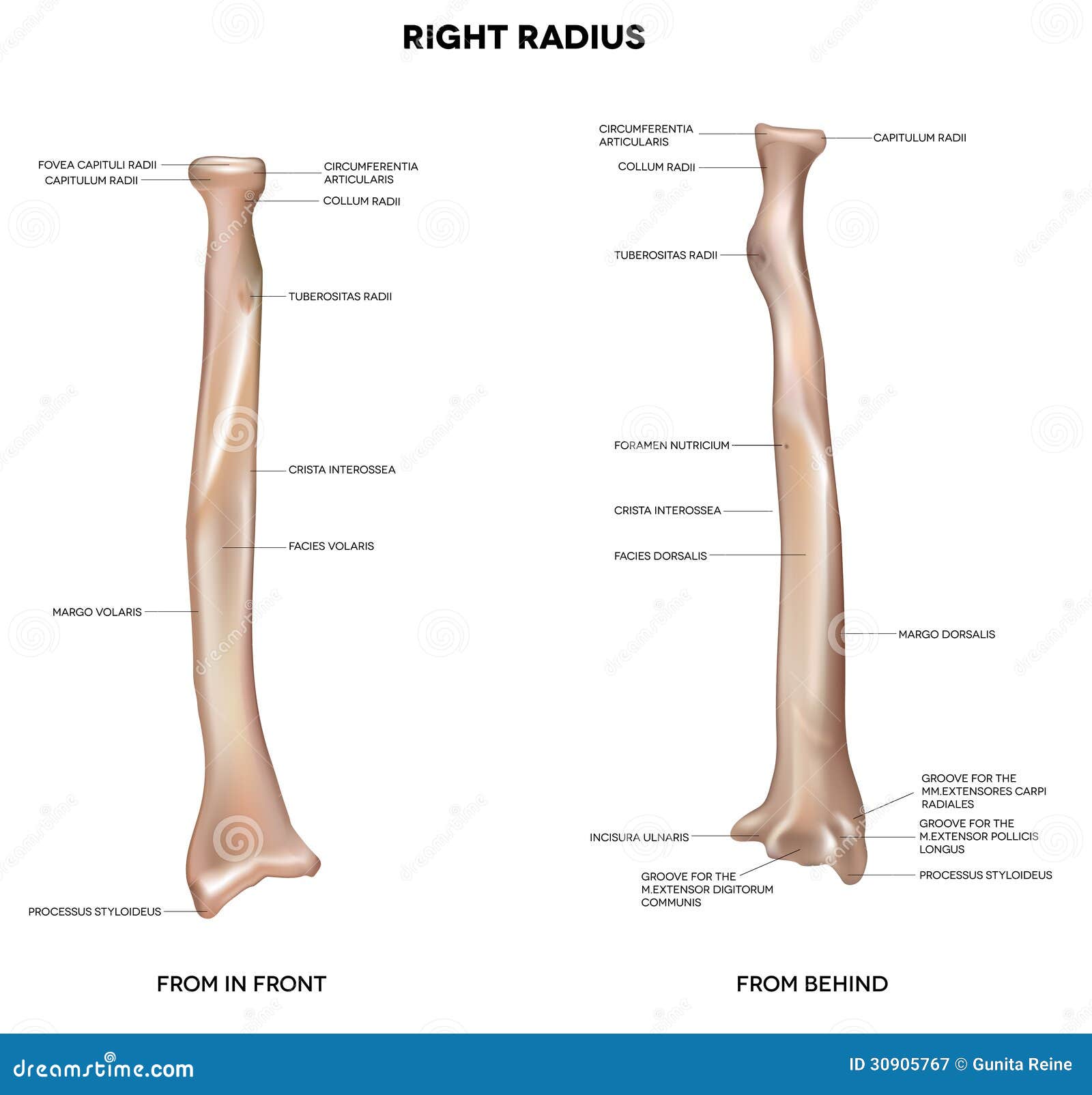
Draw a line through the centre of shaft of radius on either view. It should cut through capitellum on AP + lateral views.
4. Ossification centres
5. Radial head, olecranon, distal humerus
Supracondylar Fractures: Ortho or # Clinic
Remember a displaced anterior fat pad, any posterior fat pad or an abnormal anterior humeral line are indications of an undisplaced supracondylar fracture (or a radial head fracture) and should be treated as such with either an above elbow POP or a broad arm sling if pain is not a significant feature.
Brachial artery injury in 5-10% Type II and Type III injuries.

Radial
(~25%) and ulnar (~15%) nerve damage unlikely. 60% of median nerve
damaged. Mostly just motor branch, damaging intrinsic hand muscles so
can't flex thumb IP joint.
In your clinical examination include:
- a ‘pinch’ (medial nerve / AION),
- ‘thumbs up’ (radial nerve), and
- ‘give me four’ (finger abduction against resistance – ulnar nerve).
-
Cubitus varus (gun stock deformity)
-
Malunion and stiffness
-
Myositis ossificans
-
Nerve injury (most commonly median nerve)
-
Brachial artery (due to stretch and posterior displacement)
-
Volkmann’s ischaemic contracture (due to compartment swelling)
Manage conservatively with POP. If significant displacement, discuss with orthopaedics.
Elbow dislocation: Ortho
Elbow dislocations are surprisingly common, comprising 10 - 25% of all elbow injuries
The radial head may dislocate from the capitulum of the humerus on its own or in combination with dislocation of the ulna from the trochlea. The latter is usually straightforward to identify, but radial head dislocations may be more subtle - check the radiocapitellar line.
Radial Head: Fracture Clinic
These injuries usually follow a fall onto an outstretched wrist or direct trauma. Radial head fractures usually occur in adults and account for 30% of all adult elbow fractures. It is the second most common elbow fracture in children. Examination may reveal local bruising and swelling. In some cases pain may only be evident with palpation of the radial head during passive forearm pronation. Elbow extension is usually restricted. Assessment of the wrist should be performed due to the possibility of an Essex-Lopresti fracture-dislocation, consisting of a comminuted radial head fracture with subluxation of the distal end of the ulna.
Undisplaced fractures can be managed with a collar and cuff sling and orthopaedic outpatient follow-up. Radial neck fractures: greater than 20° of angulation in the adult or 30° in the child requires reduction.
Medial epicondyle avulsion injury: Fracture Clinic
These injuries tend to occur in adolescents due to valgus stress during a fall on an outstretched hand. There may be associated ulna nerve damage and sometimes dislocation. Undisplaced avulsions can be managed conservatively while displaced fragments should be referred for reduction.
Pulled elbow: No follow up
The radial head dislocates from the annular ligament. In 50% of cases there is no history of a pull on the arm. The x-ray is normal and therefore not necessary if clinical suspicion is high prior to attempted manipulation.
There are 2 methods for reduction;
1. Supination of the forearm followed by flexion of the elbow
2. Hyperpronation of the wrist followed by flexion of the elbow - thought to be less painful. Elbow can start at 90, or be extended. Position one hand with the thumb over the radial head.
References
http://radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_upper_limb/elbow_fracture_x-ray.html
http://www.enlightenme.org/knowledge-bank/cempaedia/elbow-injuries
http://www.enlightenme.org/learning-zone/pinch-me-thumbs-and-give-me-four
http://lifeinthefastlane.com/elbow-dislocation/
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/elbow-dislocation
http://journals.lww.com/em-news/blog/theproceduralpause/pages/post.aspx?PostID=8
http://emupdates.com/2009/09/19/emcard2054/
http://radiopaedia.org/articles/pulled-elbow-syndrome
http://emergencyeducation.net/1/post/2014/03/pulled-elbow.html
http://bestbets.org/bets/bet.php?id=123
http://pedemmorsels.com/nursemaids-elbow-feel-like-mr-miyagi/
http://www.ozemedicine.com/wiki/doku.php?id=elbow_pulled
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/supracondylar-fracture
http://emrems.com/tag/supracondylar/
http://lifeinthefastlane.com/bone-and-joint-bamboozler-007/
http://radiopaedia.org/articles/supracondylar-fracture-classification-1
http://radiopaedia.org/cases/supracondylar-process-of-humerus-1
http://radiopaedia.org/articles/olecranon-fractures-1
http://radiopaedia.org/cases/olecranon-fracture-2
http://radiopaedia.org/cases/olecranon-and-radial-head-fracture
http://radiopaedia.org/articles/radial-head-fractures