After an embarrasing handover situation, it turns out that there are guidelines for when to pull Colles fractures. I can't believe I didn't know that!
Anyway, there are normal angles to know. If the fracture doesn't meet these - it needs pulling!
Saturday, 12 July 2014
Sunday, 27 April 2014
Elbow Fractures
Radiographs
1. Anterior and posterior fat pads
- If the anterior is elevated treat it as abnormal
- If there is a posterior fat pad at all, treat as abnormal as 75% have fractures.
2. Anterior humeral line
On the lateral, draw a line down the anterior surface of the humerus. 1/3 of the capitellum should lie above the line.
3. Radiocapitellar line
Draw a line through the centre of shaft of radius on either view. It should cut through capitellum on AP + lateral views.
4. Ossification centres
As well as the bones, children have an added layer of complexity because
of the ossification centres. The ossification centres tend to appear at
these ages NOT fuse at these ages.
5. Radial head, olecranon, distal humerus
Supracondylar Fractures: Ortho or # Clinic
Remember a displaced anterior fat pad, any posterior fat pad or an abnormal anterior humeral line are indications of an undisplaced supracondylar fracture (or a radial head fracture) and should be treated as such with either an above elbow POP or a broad arm sling if pain is not a significant feature.

Complications include:
Manage conservatively with POP. If significant displacement, discuss with orthopaedics.
Elbow dislocation: Ortho
Elbow dislocations are surprisingly common, comprising 10 - 25% of all elbow injuries
The radial head may dislocate from the capitulum of the humerus on its own or in combination with dislocation of the ulna from the trochlea. The latter is usually straightforward to identify, but radial head dislocations may be more subtle - check the radiocapitellar line.
Radial Head: Fracture Clinic
These injuries usually follow a fall onto an outstretched wrist or direct trauma. Radial head fractures usually occur in adults and account for 30% of all adult elbow fractures. It is the second most common elbow fracture in children. Examination may reveal local bruising and swelling. In some cases pain may only be evident with palpation of the radial head during passive forearm pronation. Elbow extension is usually restricted. Assessment of the wrist should be performed due to the possibility of an Essex-Lopresti fracture-dislocation, consisting of a comminuted radial head fracture with subluxation of the distal end of the ulna.
Undisplaced fractures can be managed with a collar and cuff sling and orthopaedic outpatient follow-up. Radial neck fractures: greater than 20° of angulation in the adult or 30° in the child requires reduction.
Medial epicondyle avulsion injury: Fracture Clinic
These injuries tend to occur in adolescents due to valgus stress during a fall on an outstretched hand. There may be associated ulna nerve damage and sometimes dislocation. Undisplaced avulsions can be managed conservatively while displaced fragments should be referred for reduction.
Pulled elbow: No follow up
The radial head dislocates from the annular ligament. In 50% of cases there is no history of a pull on the arm. The x-ray is normal and therefore not necessary if clinical suspicion is high prior to attempted manipulation.
There are 2 methods for reduction;
1. Supination of the forearm followed by flexion of the elbow
2. Hyperpronation of the wrist followed by flexion of the elbow - thought to be less painful. Elbow can start at 90, or be extended. Position one hand with the thumb over the radial head.
References
http://radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_upper_limb/elbow_fracture_x-ray.html
http://www.enlightenme.org/knowledge-bank/cempaedia/elbow-injuries
http://www.enlightenme.org/learning-zone/pinch-me-thumbs-and-give-me-four
http://lifeinthefastlane.com/elbow-dislocation/
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/elbow-dislocation
http://journals.lww.com/em-news/blog/theproceduralpause/pages/post.aspx?PostID=8
http://emupdates.com/2009/09/19/emcard2054/
http://radiopaedia.org/articles/pulled-elbow-syndrome
http://emergencyeducation.net/1/post/2014/03/pulled-elbow.html
http://bestbets.org/bets/bet.php?id=123
http://pedemmorsels.com/nursemaids-elbow-feel-like-mr-miyagi/
http://www.ozemedicine.com/wiki/doku.php?id=elbow_pulled
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/supracondylar-fracture
http://emrems.com/tag/supracondylar/
http://lifeinthefastlane.com/bone-and-joint-bamboozler-007/
http://radiopaedia.org/articles/supracondylar-fracture-classification-1
http://radiopaedia.org/cases/supracondylar-process-of-humerus-1
http://radiopaedia.org/articles/olecranon-fractures-1
http://radiopaedia.org/cases/olecranon-fracture-2
http://radiopaedia.org/cases/olecranon-and-radial-head-fracture
http://radiopaedia.org/articles/radial-head-fractures
- If the anterior is elevated treat it as abnormal
- If there is a posterior fat pad at all, treat as abnormal as 75% have fractures.
2. Anterior humeral line
On the lateral, draw a line down the anterior surface of the humerus. 1/3 of the capitellum should lie above the line.
3. Radiocapitellar line
Draw a line through the centre of shaft of radius on either view. It should cut through capitellum on AP + lateral views.
4. Ossification centres
5. Radial head, olecranon, distal humerus
Supracondylar Fractures: Ortho or # Clinic
Remember a displaced anterior fat pad, any posterior fat pad or an abnormal anterior humeral line are indications of an undisplaced supracondylar fracture (or a radial head fracture) and should be treated as such with either an above elbow POP or a broad arm sling if pain is not a significant feature.
Brachial artery injury in 5-10% Type II and Type III injuries.

Radial
(~25%) and ulnar (~15%) nerve damage unlikely. 60% of median nerve
damaged. Mostly just motor branch, damaging intrinsic hand muscles so
can't flex thumb IP joint.
In your clinical examination include:
- a ‘pinch’ (medial nerve / AION),
- ‘thumbs up’ (radial nerve), and
- ‘give me four’ (finger abduction against resistance – ulnar nerve).
-
Cubitus varus (gun stock deformity)
-
Malunion and stiffness
-
Myositis ossificans
-
Nerve injury (most commonly median nerve)
-
Brachial artery (due to stretch and posterior displacement)
-
Volkmann’s ischaemic contracture (due to compartment swelling)
Manage conservatively with POP. If significant displacement, discuss with orthopaedics.
Elbow dislocation: Ortho
Elbow dislocations are surprisingly common, comprising 10 - 25% of all elbow injuries
The radial head may dislocate from the capitulum of the humerus on its own or in combination with dislocation of the ulna from the trochlea. The latter is usually straightforward to identify, but radial head dislocations may be more subtle - check the radiocapitellar line.
Radial Head: Fracture Clinic
These injuries usually follow a fall onto an outstretched wrist or direct trauma. Radial head fractures usually occur in adults and account for 30% of all adult elbow fractures. It is the second most common elbow fracture in children. Examination may reveal local bruising and swelling. In some cases pain may only be evident with palpation of the radial head during passive forearm pronation. Elbow extension is usually restricted. Assessment of the wrist should be performed due to the possibility of an Essex-Lopresti fracture-dislocation, consisting of a comminuted radial head fracture with subluxation of the distal end of the ulna.
Undisplaced fractures can be managed with a collar and cuff sling and orthopaedic outpatient follow-up. Radial neck fractures: greater than 20° of angulation in the adult or 30° in the child requires reduction.
Medial epicondyle avulsion injury: Fracture Clinic
These injuries tend to occur in adolescents due to valgus stress during a fall on an outstretched hand. There may be associated ulna nerve damage and sometimes dislocation. Undisplaced avulsions can be managed conservatively while displaced fragments should be referred for reduction.
Pulled elbow: No follow up
The radial head dislocates from the annular ligament. In 50% of cases there is no history of a pull on the arm. The x-ray is normal and therefore not necessary if clinical suspicion is high prior to attempted manipulation.
There are 2 methods for reduction;
1. Supination of the forearm followed by flexion of the elbow
2. Hyperpronation of the wrist followed by flexion of the elbow - thought to be less painful. Elbow can start at 90, or be extended. Position one hand with the thumb over the radial head.
References
http://radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_upper_limb/elbow_fracture_x-ray.html
http://www.enlightenme.org/knowledge-bank/cempaedia/elbow-injuries
http://www.enlightenme.org/learning-zone/pinch-me-thumbs-and-give-me-four
http://lifeinthefastlane.com/elbow-dislocation/
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/elbow-dislocation
http://journals.lww.com/em-news/blog/theproceduralpause/pages/post.aspx?PostID=8
http://emupdates.com/2009/09/19/emcard2054/
http://radiopaedia.org/articles/pulled-elbow-syndrome
http://emergencyeducation.net/1/post/2014/03/pulled-elbow.html
http://bestbets.org/bets/bet.php?id=123
http://pedemmorsels.com/nursemaids-elbow-feel-like-mr-miyagi/
http://www.ozemedicine.com/wiki/doku.php?id=elbow_pulled
http://academiclifeinem.com/tricks-of-the-trade-nursemaid-elbow-reduction/
http://radiopaedia.org/articles/supracondylar-fracture
http://emrems.com/tag/supracondylar/
http://lifeinthefastlane.com/bone-and-joint-bamboozler-007/
http://radiopaedia.org/articles/supracondylar-fracture-classification-1
http://radiopaedia.org/cases/supracondylar-process-of-humerus-1
http://radiopaedia.org/articles/olecranon-fractures-1
http://radiopaedia.org/cases/olecranon-fracture-2
http://radiopaedia.org/cases/olecranon-and-radial-head-fracture
http://radiopaedia.org/articles/radial-head-fractures
Tuesday, 8 April 2014
Forearm Fractures
 It's difficult to separate the radius from the ulnar as you progress up the forearm but isolated fractures can occur. Forearm fractures frequently seen in school aged children after a fall. Adult fractures may be markedly displaced with little or no bony contact between the fragments. ORIF needed
It's difficult to separate the radius from the ulnar as you progress up the forearm but isolated fractures can occur. Forearm fractures frequently seen in school aged children after a fall. Adult fractures may be markedly displaced with little or no bony contact between the fragments. ORIF needed Isolated ulnar fracture
Rare but can happen if the arm is in a defensive position, as in martial arts. POP. If displaced or angulated, for ORIF.
Isolated radial fracture
Very rare
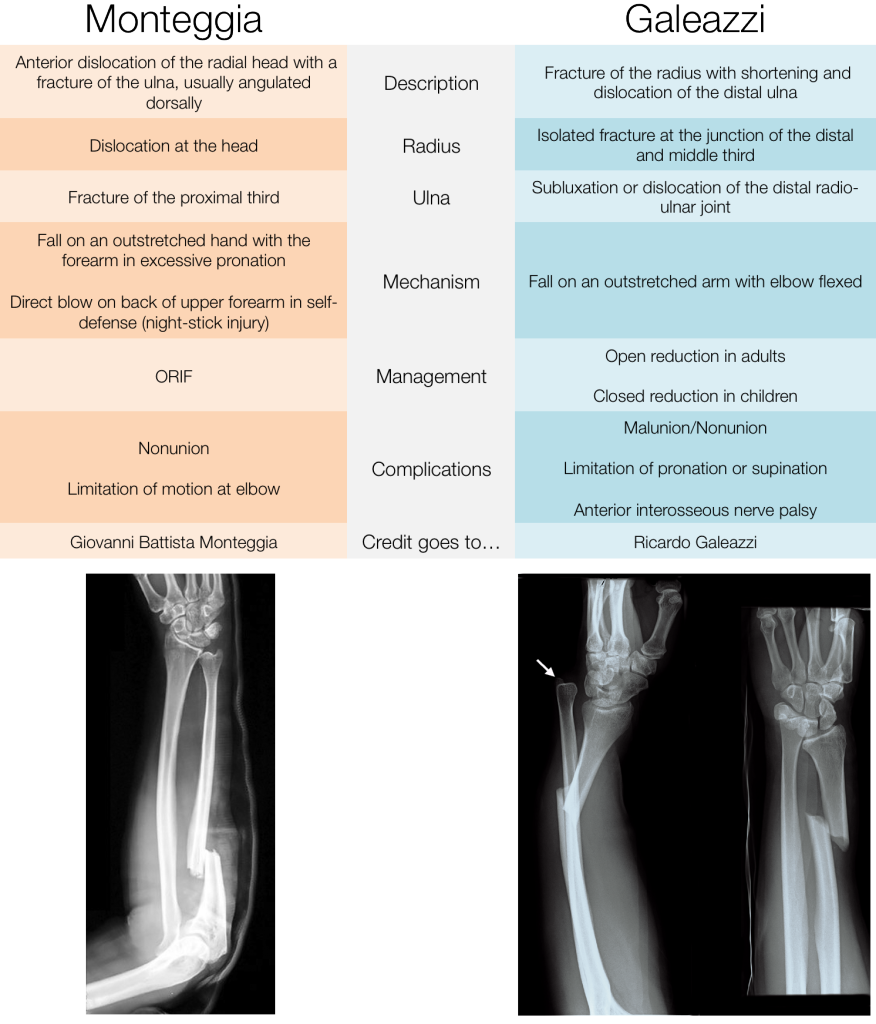
Monteggia Fracture


Ulnar fracture and radial dislocation. You need to look carefully at the radiocapitella line. If it does not transect the middle of the capitlellum, there is a radial head dislocation. Occurs by forced pronation of the outstretched forarm. Urgent ORIF needed.

Galeazzi - radial fracture, dislocation at distal radioulnar joint. This occurs in teenagers and is very rare.
 |
| http://www.pemcincinnati.com/blog/fracture-fridays-monteggiazzi/ |
" MUGR (Mugger): Monteggia Fracture = Ulnar fracture with radial head dislocation; Galeazzi Fracture = Radius fracture with DRUJ dislocation."
Monday, 7 April 2014
The Radius
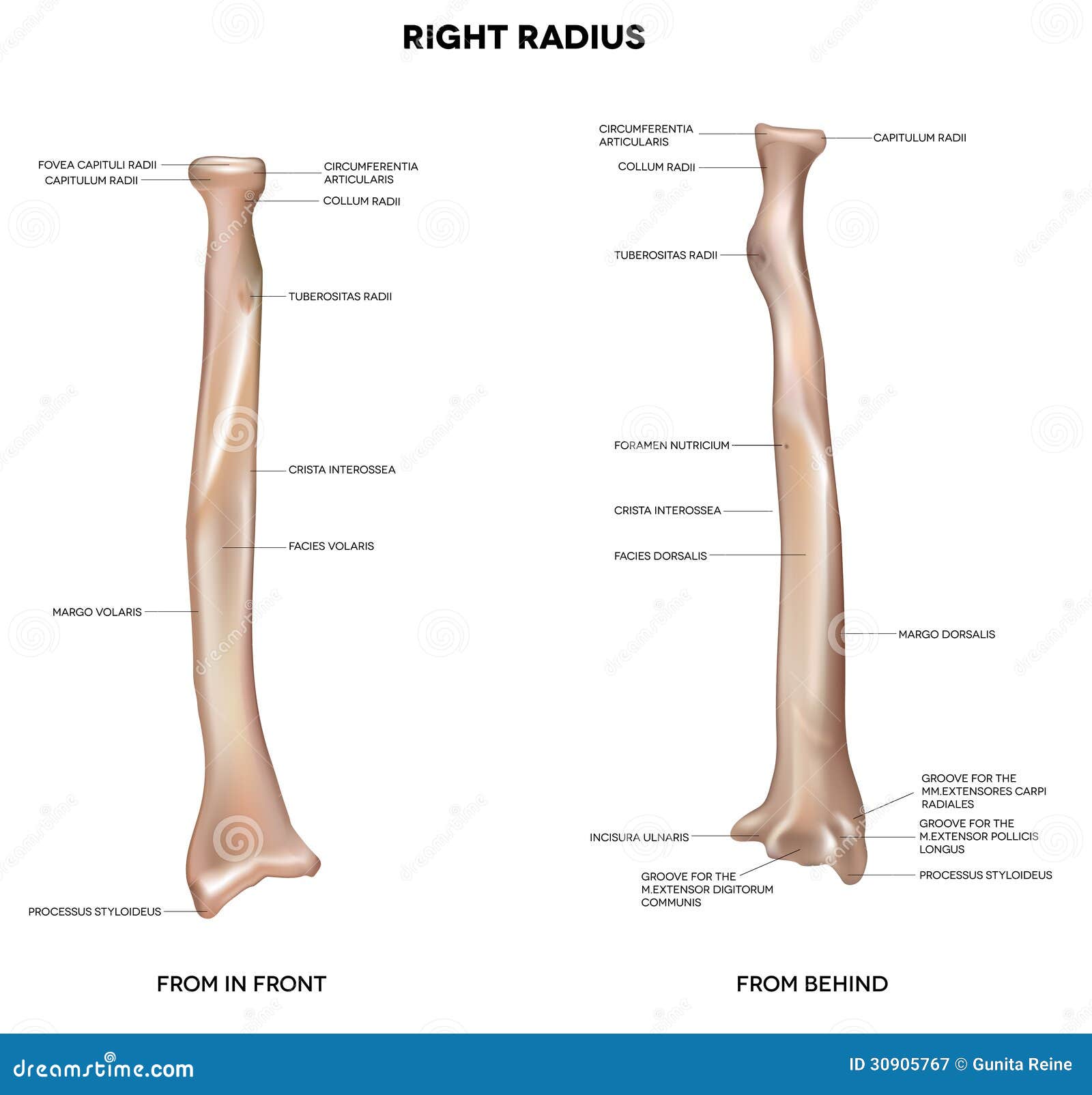
The radius is commonly fractured at the wrist. Because of the close connections with the ulna, breaks often happen together - at the wrist, the radius is the bone that is important, and is used to categorise the break.
Colles Fracture
 Radius within 2.5cm of the wrist. Distal fragment angulated to point dorsally.
Radius within 2.5cm of the wrist. Distal fragment angulated to point dorsally.Analgesia, POP, elevation
Discharge undisplaced
Complications: stiffness, malunion, reflex sympathetic dystrophy (Sudeck's atrophy) - refer for physiotheraphy, carpal tunnel syndrome, extensor pollicis longus rupture
Smith's Fracture
Unstable distal radius fracture (or reverse Colles' fracture)
The distal fragment is impacted, tilted anteriorly.
From a fall onto a flexed wrist.
Analgesia, POP, orthopaedics
The distal fragment is impacted, tilted anteriorly.
From a fall onto a flexed wrist.
Analgesia, POP, orthopaedics
Barton's Fracture
Intra-articular fracture involving the volar portion of the distal radius. The resultant fragment slips anteriorly, so the fracture is unstable.
POP and refer
POP and refer
http://radiopaedia.org/articles/colles-fracture
http://emergencymedicineireland.com/2012/05/anatomy-for-emergency-medicine-17-colles-fractures/
http://emrems.com/tag/colles/
http://emj.bmj.com/content/29/9/781.2.extract
http://radiopaedia.org/cases/distal-radial-fracture-colles-fracture-1
http://blog.ercast.org/2011/07/distal-radial-fractures/
http://radiopaedia.org/cases/colles-fracture-1
http://radiopaedia.org/cases/colles-fracture-6
http://www.ajemjournal.com/article/S0735-6757%2809%2900492-6/abstract
Smith's Fracture
http://www.enlightenme.org/learning-zone/when-colles%E2%80%99-not-colles%E2%80%99
http://radiopaedia.org/articles/smith-fracture
http://radiopaedia.org/cases/smith-fracture
Barton's Fracture
http://lifeinthefastlane.com/bone-and-joint-bamboozler-003/
The Carpal Bones
 |
| http://www.instantanatomy.net/arm/areas/hand/carpalbones.html |
Fractures are 10 times less likely to occur than distal radial and ulnar injuries and are rare in children under 12. Injuries more likely in the proximal carpal row (scaphoid, lunate, triqetrum, pisiform).
TriquetrumThis is the second most fractured carpal bone accounting for 20%Z of carpal injuries. May be related to forced hyperextension. Normally seen as small triangular fragements or flake avulsions.
Treat with immobilisation in a POP backslab or wrist support splint, analgesia and refer to fracture clinic.
HamateThis is often caused by axial loading or punch type injury. Suspect if there is local palmar tenderness. Diagnosis can be difficult.
LunateFractures are uncommon, and mechanism is typically a direct blow to the carpus. Avascular necrosis may occur.
Pisiform
Direct blow or FOOSH.
Capitate
Axial loading of the middle metacarpal. Often missed.
Trapezoid
Rare. Axial loading of the index metacarpal.
Trapezium
Rare. Forced abduction of the thumb. Can mimic a scaphoid fracture.
All of these injuries should be referred to plastics?
http://www.memrise.com/course/59292/anatomy-of-the-hand/
Olecranon Fractures
 The Olecranon is the proximal part of the humerus. It is rare to fracture it. Olecranon fractures usually occur after
The Olecranon is the proximal part of the humerus. It is rare to fracture it. Olecranon fractures usually occur after- direct blow or fall onto the elbow
- fall on outstretched hand with elbow flexed
- avulsion fracture
- stress fracture eg. throwing, weight lifting
Clinical Features
Significant amounts of elbow swelling
Inability to extend arm (due to triceps rupture)
Ulnar nerve injury possible
Fracture is normally obvious.
The radiological difficulty is differentiating fractures from the olecranon epiphysis. The olecranon epiphysis appears between the age of 8 and 11, and fuses by the age of 14.
Management
Undisplaced needs above elbow backslab, and fracture clinic.
Displaced or involving then elbow joint need an ORIF - so immediate orthopaedic opinion.
References
http://radiopaedia.org/articles/olecranon-fractures-1
http://radiopaedia.org/cases/olecranon-fracture-2
Oxford Handbook of Emergency Medicine
Minor Injuries
Musculoskeletal Trauma
Emergency Care of Minor Trauma in Children
Sunday, 6 April 2014
Scaphoid Fractures
There's loads of really good FOAMEd resources out there already about scaphoid fractures. It's common (2-7% of all fractures), and most commonly occurs in young people as result of FOOSH.
Anatomy - look at Emergency Medicine Ireland. It's fabulous, why do anything else?
Clinical Examination
Clinical examination is rubbish, but a combination of ASB tenderness (90% sensitivity, 40% specificity), thumb axial compression and scaphoid tubercle tenderness (57% specificity) is the best way.
Imaging
You might see:
- visualisation of the fracture +/- displacement
- soft tissue swelling and lateral displacement of the adjacent fat pads
- scaphoid fat pad sign - formation of a straight/convex line adjacent to the concave aspect of the scaphoid
- associated scapholunate ligament disruption (Terry Thomas sign)
Helpfully, 25-30% have normal x-rays.
Ultrasound is not sensitive enough. Most places go for CT or MRI.
Management
If radiologically confirmed, no displacement, POP and fracture clinic.
Distal 1/3 - 6-8 weeks.
Middle 1/3 – 8-12 weeks.
Proximal 1/3 – 12-23 weeks.
If radiologically confirmed + displacement, speak to plastics.
If no radiological evidence, splint and bring back to fracture clinic. Thumb extension is not needed, as long as there is no ulnar deviation.
Complications
Avascular necrosis occurs in 30-40% of untreated fractures. It is less than 10% in undisplaced fractures. Non-union occurs in 5-12% of treated fractures, and the incidence of complications increases with proximal pole fractures.
80% of patients are immobilised unnecessarily.
References
http://www.enlightenme.org/knowledge-bank/cem-ctr/early-ct-clinically-suspected-scaphoid-fractures
http://bestbets.org/bets/bet.php?id=2003
http://bestbets.org/bets/bet.php?id=1687
http://bestbets.org/bets/bet.php?id=1673
http://lifeinthefastlane.com/scaphoid-fractures-the-ed-perspective/
http://emergencymedicineireland.com/2012/06/anatomy-for-emergency-medicine-19-scaphoid-fractures/
http://blogs.bmj.com/bjsm/2013/12/16/current-management-of-occult-scaphoid-fractures-in-uk-emergency-departments/
http://radiopaedia.org/articles/scaphoid_fracture
http://foam4gp.com/2013/11/15/foam4gp-map-scaphoid-fractures-thumbing-through-the-research/
http://radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_upper_limb/wrist_trauma_x-ray.html
http://shortcoatsinem.blogspot.co.uk/2012/03/heeling-scaphoid-terrible-pun-intended.html
Anatomy - look at Emergency Medicine Ireland. It's fabulous, why do anything else?
Clinical Examination
Clinical examination is rubbish, but a combination of ASB tenderness (90% sensitivity, 40% specificity), thumb axial compression and scaphoid tubercle tenderness (57% specificity) is the best way.
Imaging
You might see:
- visualisation of the fracture +/- displacement
- soft tissue swelling and lateral displacement of the adjacent fat pads
- scaphoid fat pad sign - formation of a straight/convex line adjacent to the concave aspect of the scaphoid
- associated scapholunate ligament disruption (Terry Thomas sign)
Helpfully, 25-30% have normal x-rays.
Ultrasound is not sensitive enough. Most places go for CT or MRI.
Management
If radiologically confirmed, no displacement, POP and fracture clinic.
Distal 1/3 - 6-8 weeks.
Middle 1/3 – 8-12 weeks.
Proximal 1/3 – 12-23 weeks.
If radiologically confirmed + displacement, speak to plastics.
If no radiological evidence, splint and bring back to fracture clinic. Thumb extension is not needed, as long as there is no ulnar deviation.
Complications
Avascular necrosis occurs in 30-40% of untreated fractures. It is less than 10% in undisplaced fractures. Non-union occurs in 5-12% of treated fractures, and the incidence of complications increases with proximal pole fractures.
80% of patients are immobilised unnecessarily.
References
http://www.enlightenme.org/knowledge-bank/cem-ctr/early-ct-clinically-suspected-scaphoid-fractures
http://bestbets.org/bets/bet.php?id=2003
http://bestbets.org/bets/bet.php?id=1687
http://bestbets.org/bets/bet.php?id=1673
http://lifeinthefastlane.com/scaphoid-fractures-the-ed-perspective/
http://emergencymedicineireland.com/2012/06/anatomy-for-emergency-medicine-19-scaphoid-fractures/
http://blogs.bmj.com/bjsm/2013/12/16/current-management-of-occult-scaphoid-fractures-in-uk-emergency-departments/
http://radiopaedia.org/articles/scaphoid_fracture
http://foam4gp.com/2013/11/15/foam4gp-map-scaphoid-fractures-thumbing-through-the-research/
http://radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_upper_limb/wrist_trauma_x-ray.html
http://shortcoatsinem.blogspot.co.uk/2012/03/heeling-scaphoid-terrible-pun-intended.html
Abdominal and Orbital Compartment Syndrome
Abdominal compartment syndrome often follows laparotomy. Tissue swelling combined with packing or haematomas may cause rising abdominal pressures, causing cardiovascular, respiratory, renal and cerebral dysfunction.
It is best noticed by a fall in urine output + raised JVP
Increased Risk If:
Diminished Abdominal Wall Compliance
acute respiratory failure (especially with elevated intrathoracic pressure)
abdominal surgery with fascial closure
major trauma/burns
prone positioning
head > 30 degrees
high BMI
central obesity
Increased Intra-luminal Contents
gastroparesis
ileus
colonic pseudo-obstruction
Increased Abdominal Contents
haemo/pneumoperitoneum
ascites
liver dysfunction
Capillary Leak or Fluid Resuscitation
acidosis (pH < 7.2)
hypotension
hypothermia (T < 33 C)
massive transfusion (> 10 U in 24 hrs)
coagulopathy
massive fluid resuscitation
pancreatitis
sepsis
oliguria
damage control laparotomy
Retrobulbar hemorrhage with acute orbital compartment syndrome is primarily a clinical diagnosis. CT may show a diffuse, increased reticular pattern of the intraconal orbital fat rather than a discrete hematoma.
A teardrop or tenting sign is ominous - it occurs when the optic nerve is at maximum stretch and distorts the back of the globe into a teardrop shape.
The main steps in emergency canthotomy/ cantholysis are:
use local anesthetic but warn the patient that they may feel pain
Perform the canthotomy:
place the scissors across the lateral canthus and incise the canthus full thickness
Perform cantholysis:
Grasp the lateral lower eyelid with toothed forceps
Pull the lower eyelid anteriorly
Point the scissors toward the patient’s nose, place the blades either side of the lateral canthal tendon, and cut
http://ccforum.com/content/4/1/23
http://lifeinthefastlane.com/ophthalmology-befuddler-033-2/
It is best noticed by a fall in urine output + raised JVP
Increased Risk If:
Diminished Abdominal Wall Compliance
acute respiratory failure (especially with elevated intrathoracic pressure)
abdominal surgery with fascial closure
major trauma/burns
prone positioning
head > 30 degrees
high BMI
central obesity
Increased Intra-luminal Contents
gastroparesis
ileus
colonic pseudo-obstruction
Increased Abdominal Contents
haemo/pneumoperitoneum
ascites
liver dysfunction
Capillary Leak or Fluid Resuscitation
acidosis (pH < 7.2)
hypotension
hypothermia (T < 33 C)
massive transfusion (> 10 U in 24 hrs)
coagulopathy
massive fluid resuscitation
pancreatitis
sepsis
oliguria
damage control laparotomy
Orbital Compartment Syndrome
Retrobulbar hemorrhage with acute orbital compartment syndrome is primarily a clinical diagnosis. CT may show a diffuse, increased reticular pattern of the intraconal orbital fat rather than a discrete hematoma.
A teardrop or tenting sign is ominous - it occurs when the optic nerve is at maximum stretch and distorts the back of the globe into a teardrop shape.
The main steps in emergency canthotomy/ cantholysis are:
use local anesthetic but warn the patient that they may feel pain
Perform the canthotomy:
place the scissors across the lateral canthus and incise the canthus full thickness
Perform cantholysis:
Grasp the lateral lower eyelid with toothed forceps
Pull the lower eyelid anteriorly
Point the scissors toward the patient’s nose, place the blades either side of the lateral canthal tendon, and cut
http://ccforum.com/content/4/1/23
http://lifeinthefastlane.com/ophthalmology-befuddler-033-2/
Compartment Syndrome
Compartment syndrome is without doubt one of the diagnoses that we should never miss. Palpable distal pulses and normal capillary refill times do not exclude compartment syndrome.
Pathophysiology
The pressure inside a body compartment increases. The compartment can't compensate for the increase in pressure, so puts pressure on nerves and blood vessels, making limbs painful and ischaemic.
Compartment syndrome can affect many regions of the body and is more common in:
- the forearm (volar compartment): humeral shaft fracture, radius and ulna fracture, supracondylar fracture
- leg (the anterior compartment): tibia fracture
It can occur in other regions, including the back, buttocks, thigh, abdomen and foot. Compartment syndrome of the deep posterior compartment of the leg is easily missed.
Compartment syndrome can also occur after soft tissue injuries:
crush injury
snake bite
excessive exertion and exercise - used to be called anterior tibial syndrome. Pain persists despite rest.
prolonged immobilisation
constrictive dressings and plaster casts
soft tissue infection
seizures
extravasation of intravenous fluids and medications
burns
tourniquets
Patients with a coagulopathy are at particular risk of compartment syndrome.
DiagnosisSuspicion is essential! Suspect if:
- one of the fractures listed above is present
- one of the soft tissue injuries listed above is present (e.g. crush injury)
- patient has a coexistent coagulopathy
Examination - The 6Ps 1. pain - Occurs early, is persistent, tends to be disproportionate compared with the original injury and is not relieved by immobilisation. Passive stretching worsens the pain.
2. pallor
3. perishingly cold
4. pulselessness (a late sign)
5. paralysis
6. paraesthesiae - assess by light touch and two-point discrimination, rather than just pinprick, which is less sensitive.
The extremity may be swollen and affected compartments may feel tense and tender on palpation.
Pressures:
zero - 10 mmHg = normal tissue pressure
>20mmHg = capillary blood flow may be compromised
>30 - 40mmgHg = muscle and nerve fibers at risk for ischemic necrosis at pressures
Thinking about the Whiteside' Theory:
"the development of a compartment syndrome depends not only on intra-compartment pressure but also depends on systemic blood pressure" treatment may depend on calculating the delta pressure.
Delta pressure = diastolic blood pressure (DBP) — intracompartment pressure
A delta pressure <30 mmHg is suggestive of compartment syndrome
Treatment
This is a surgical / orthopaedic emergency - ischemic injury to muscles and nerves occurs after 4 hours of complete ischemia and becomes irreversible over the next 4 hours, resulting in local rhabdomyolysis and neuropraxis.
Remove all constrictive dressings
Elevation
Traction as appropriate
Analgesia
IV hydration to relieve rhabdomyolysis
References
http://lifeinthefastlane.com/ortho-library/compartment-syndrome/
http://radiopaedia.org/articles/chronic-exertional-compartment-syndrome
http://www.bmj.com/content/325/7364/557?sso=
http://www.trauma.org/archive/resus/DCSacs.html
http://lifeinthefastlane.com/bone-and-joint-bamboozler-002/
http://lifeinthefastlane.com/education/ccc/abdominal-compartment-syndrome/
http://journals.lww.com/anesthesia-analgesia/Fulltext/1996/12000/Acute_Biceps_Compartment_Syndrome_Associated_with.40.aspx
http://bjsm.bmj.com/content/38/2/218.full
http://pedemmorsels.com/compartment-syndrome/
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Acute%20Compartment%20Syndrome.jpg
Pathophysiology
The pressure inside a body compartment increases. The compartment can't compensate for the increase in pressure, so puts pressure on nerves and blood vessels, making limbs painful and ischaemic.
Compartment syndrome can affect many regions of the body and is more common in:
- the forearm (volar compartment): humeral shaft fracture, radius and ulna fracture, supracondylar fracture
- leg (the anterior compartment): tibia fracture
It can occur in other regions, including the back, buttocks, thigh, abdomen and foot. Compartment syndrome of the deep posterior compartment of the leg is easily missed.
Compartment syndrome can also occur after soft tissue injuries:
crush injury
snake bite
excessive exertion and exercise - used to be called anterior tibial syndrome. Pain persists despite rest.
prolonged immobilisation
constrictive dressings and plaster casts
soft tissue infection
seizures
extravasation of intravenous fluids and medications
burns
tourniquets
Patients with a coagulopathy are at particular risk of compartment syndrome.
DiagnosisSuspicion is essential! Suspect if:
- one of the fractures listed above is present
- one of the soft tissue injuries listed above is present (e.g. crush injury)
- patient has a coexistent coagulopathy
Examination - The 6Ps 1. pain - Occurs early, is persistent, tends to be disproportionate compared with the original injury and is not relieved by immobilisation. Passive stretching worsens the pain.
2. pallor
3. perishingly cold
4. pulselessness (a late sign)
5. paralysis
6. paraesthesiae - assess by light touch and two-point discrimination, rather than just pinprick, which is less sensitive.
The extremity may be swollen and affected compartments may feel tense and tender on palpation.
Pressures:
zero - 10 mmHg = normal tissue pressure
>20mmHg = capillary blood flow may be compromised
>30 - 40mmgHg = muscle and nerve fibers at risk for ischemic necrosis at pressures
Thinking about the Whiteside' Theory:
"the development of a compartment syndrome depends not only on intra-compartment pressure but also depends on systemic blood pressure" treatment may depend on calculating the delta pressure.
Delta pressure = diastolic blood pressure (DBP) — intracompartment pressure
A delta pressure <30 mmHg is suggestive of compartment syndrome
Treatment
This is a surgical / orthopaedic emergency - ischemic injury to muscles and nerves occurs after 4 hours of complete ischemia and becomes irreversible over the next 4 hours, resulting in local rhabdomyolysis and neuropraxis.
Remove all constrictive dressings
Elevation
Traction as appropriate
Analgesia
IV hydration to relieve rhabdomyolysis
References
http://lifeinthefastlane.com/ortho-library/compartment-syndrome/
http://radiopaedia.org/articles/chronic-exertional-compartment-syndrome
http://www.bmj.com/content/325/7364/557?sso=
http://www.trauma.org/archive/resus/DCSacs.html
http://lifeinthefastlane.com/bone-and-joint-bamboozler-002/
http://lifeinthefastlane.com/education/ccc/abdominal-compartment-syndrome/
http://journals.lww.com/anesthesia-analgesia/Fulltext/1996/12000/Acute_Biceps_Compartment_Syndrome_Associated_with.40.aspx
http://bjsm.bmj.com/content/38/2/218.full
http://pedemmorsels.com/compartment-syndrome/
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Acute%20Compartment%20Syndrome.jpg
Friday, 28 February 2014
Finger Injuries
HistoryRemember to check left or right -handed ness, occupation, and social situation
Documentation
Refer to fingers by name not number.
Use palmar (or volar), dorsal, radial, ulnar (not anterior, posterior, lateral, medial).
Document important positives, as well as important negatives
Examination
Remove rings as soon as possible
X-ray if any likelihood of glass
ElevationThe importance of elevation can not be emphasised enough. The injured hand must always be higher than the heart. Many complications from hand injuries are not from the fracture and associated soft tissue, but from persistent oedema - making healing slower, and surgery more difficult. Elevate!
HealingA fracture in the hand takes 4 weeks to heal clinically, and is faster in children. Radiographic healing can take 4 - 6 months. They begin to heal 7 days after injury. Attempts at closed manipulation after 7 days in children, and adults in 10 days are usually unsuccessful.
Hands should be seen by the specialist less than 5 days after the initial injury.
Tendon InjuriesExtensor Tendon Injuries: Plastics Extensor tendon injuries can be just as devastating as flexor tendon injuries. If suspected, whether partial or full, refer the patient to plastic surgeons. If the injury is less than 50%, conservative management may be considered. A mallet splint should be applied, even if no deformity is apparent.
A mallet finger is loss of extensive extension of the distal interphalangeal joint caused by failure of the terminal slip of the extensor mechanism at its insertion. It is often caused when the extended finger is accidentally stubbed against a hard surface. They should be x-rayed to see whether there is an avulsion fracture present - bony injury is a good prognostic indicator.
Large bony fragment (>1/3 articular surface) = mallet splint + speedy plastics review.
No bony fragment = plastics review clinic 7 - 10 days
Subluxation = speedy plastics review
Flexor Tendon Injuries: PlasticsThere is some controversy about whether to repair these or not. Lacerations can cause flexor tendon injuries, and avulsions from the base of the distal phalynx are commonly missed.
“Rugby shirt finger” is more common in adolescence, and commonly affects the ring finger. Forced extension of the distal phalanx (as in grabbing someone’s collar at rugby) tears the FDP tendon. They can be difficult to diagnose, and a high index of suspicion from the history is needed. They require surgery in <10 days.
Ulnar Collateral Ligament: Plastics The UCL can be ruptured by forced abduction - nowadays from falling when skiing onto the ski-pole. It used to be caused by gamekeeping injuries. The eponymous name “Gamekeeper’s thumb” is being replaced by “Skiiers thumb”. Complete rupture is when the two parts of ligament being separated by the adductor aponeursis (the Stener lesion”).
UCL Sprains: Sometimes the UCL is sprained, and it can be difficult to assess for laxity due to pain. Some texts suggest anaesthetising the UCL and re-assessing. If you are unable to assess the UCL and have a high index of suspicion, treat as per rupture and refer the patient to plastics clinic follow up. If you are unable to assess the UCL and have a low index of suspicion, refer the patient to UCC follow up clinic.
UCL Laxity: If there is laxity >30 degrees, refer the patient to plastics. The thumb should be immobilised in thumb-spica - either tape or plaster of paris.
Avulsion fracture: a UCL sprain or rupture + avulsion fracture should be treated with a scaphoid plaster of paris, and plastics referral.
Nerve InjuriesDigital Nerve Injury: PlasticsThe digital nerve can easily be damaged, and often sensation is intact, but altered. Complaints of altered sensation should be taken seriously.
It is important to have sensation over the edges of the hand - the thumb, the radial aspect of the index finger, or ulnar aspect of the little finger. Repair can be successful up to 2 weeks after injury.
The digital nerves can be repaired up to the level of the DIPJ, although it may be decided not to repair injuries distal to the PIPJ.
When examining the finger for suspected digital nerve damage, it can be useful to test for tactile adherence by running a bic biro along the finger. If there is nerve injury, the biro will slide a lot more easily than normal. It should be a bic biro used as other biros do not have the smooth surface required. Soft Tissue Injuries
Amputations: PlasticsAny amputations, even if there is only a small part amputated should be x-rayed, dressed, bandaged and elevated. Give analgesia, tetanus cover and, broad spectrum antibiotics.
Wrap the amputated part in moist saline swabs and place in a sealed plastic bag surrounded by ice/water mix at 4 degrees.
Amputations should be referred urgently to plastics. If there is problem obtaining haemostasis, and ED seniors can not help, urgent orthopaedic help may be needed.
Finger pad amputations: PlasticsFinger pad amputations are common, especially in children. If skin loss is <1cm2 without bony exposure it may be allowed to heal with non-stick dressings. Larger areas of loss may require grafting. Even if they are small, these wounds need regular follow up and are best followed up in the plastic clinic.
Crush injuries: UCC Review Clinic or GPCrush injuries often cause “burst” injury of fingertip wounds. They should be cleaned, and then closed as appropriate. Remember the wound is likely to swell, so closure can be difficult.
Most of the time these injuries can be reviewed by the GP or Practice Nurse. If you suspect blunt tendon rupture, they need review in plastics clinic. If the area of crush is significant, plastics must be involved.
High pressure injection injuries: PlasticsRefer for immediate exploration and debridement, even if the injury appears minor.
Pulp Infections: GPRemember to X-ray to look for a foreign object or osteomyelitis. Incise over the point of maximal fluctuence, and send the patient home with oral antibiotics (flucloxacillin) and wound care advice.
Pyogenic flexor tenosynovitis: PlasticsKanavel’s signs: tenderness over the flexor tendon, symmetrical swelling of the finger, finger held in flexion, pain on passive extension
Refer for exploration, irrigation, and IV antibiotics.
Phalanx FracturesDistal phalynx fracture (closed): GP/ plasticsAnalgesia and elevation. Buddy strap for symptomatic relief.
These heal well, and do not need orthopaedic or plastic follow up, unless they are complicated. In children, if the fracture is through the growth plate the injury should be followed up by plastics.
Distal phalynx fracture (open): PlasticsThis counts as a complicated fracture and should be referred to plastics for consideration of exploration.
Simple proximal and middle phalangeal fractures: GPThese should be treated with excellent elevation, neighbour strapping and analgesia. Unless requiring manipulation, they do not need follow up. Make sure you have a good lateral to assess the degree of rotation or angulation.
Complicated proximal and middle phalangeal fractures: plasticsAny angulated phalynx fractures should be manipulated - use a needle-holder or pencil placed adjacent to the web space as a fulcrum. You may need to maintain reduction with a volar slap or a Zimmer splint.
Refer speedily for surgical fixation if reduction is unsatisfactory or can not be maintained.
Phalangeal Dislocations: plasticsAlways X-ray before reduction and then reduce under digital nerve block or entonox with traction and gentle manipulation. Check integrity of the collateral ligaments after reduction. Buddy strap, elevate, analgesia and provide follow up. Metacarpal fractures
The management of a metacarpal fracture depends on which bit of the metacarpal, which finger, and how angulated it is. Elevation is the most important component of treatment!
Metacarpal Head: PlasticsApply a volar slab, encourage elevation, and refer to plastics.
Metacarpal Neck and Shaft: plasticsCarefully assess degree of rotation and then apply a volar slab or ulnar gutter. Encourage elevation. Most fractures are treated non-operatively, especially in the middle and index metacarpal.
Refer acutely for operative intervention if any rotational deformity, more than 5mm shortening or more than 10o, 10o, 20o, 20o of angulation respectively for 2nd - 5th metacarpals.
Metacarpal Base: plasticsCheck lateral x-ray carefully to ensure the carpo-metacarpal joint is not dislocated, as metacarpal base fractures are frequently fracture-dislocations. These are typically unstable and should be treated with a volar slab or ulnar gutter, elevated, and referred to plastics.
Thumb Base fractures: plasticsIntrarticular: Bennett’s (fracture fragment on ulnar side of thumb)
Rolando (fracture fragment on radial side of thumb)
Apply a bennett’s POP (like a scaphoid but thumb abducted) and refer to plastics for speedy operative repair.
Extraarticular: Check dorsal angulation. If angulated more than 30o or shortened more than 4mm, need speedy operative repair. If non-angulated, refer to plastics for follow up.
Thumb dislocations: plasticsReduce thumb dislocations, then immobilise in a scaphoid POP + follow up.
.
Little (5th) MC dislocation: plasticsMay be associated with fracture - refer after reduction for internal fixation.
MCPJ Dislocation: plasticsAfter reduction assess integrity of collateral ligaments. Then immobilise in 15 degree flexion. If failed reduction, refer for open reduction
Other Hand ProblemsVolar plate injury: plasticsHyperextension at the PIPJ injures the volar plate at the base of the middle phalanx without evidence of bony involvement. Examination shows fusiform swelling of the PIPJ with tenderness over the volar aspect. Treat with buddy strapping to adjacent fingers. Plastics review needed to ensure full mobility regained.
Locked Finger: plasticsThis is common in elderly patients with osteoarthritis. There is often no history of trauma. Refer for hand surgeon opinion - do not try to straighten the affected finger.
Trigger finger/ thumb: GPSpecialist to inject steroid injection into the flexor tendon sheath. GP to refer to orthopaedics.
Fight Bite: PlasticsSuspect a fight bite in any patient presenting with wounds on the dorsum of the hand over the index, middle, ring or little finger MC heads of having sustained a human bite, what ever history is given. Many plastic surgery centres will thoroughly irrigate all of these wounds in theatre, so discuss them all.
Reading and References
http://academiclifeinem.com/pv-card-metacarpal-fractures/
http://learning.bmj.com/learning/module-intro/managing-minor-skiing-snowboarding-injuries-primary-care.html?moduleId=5003325&searchTerm=%E2%80%9Chand%E2%80%9D&page=3&locale=en_GB
https://gmep.org/media/13991
http://lifeinthefastlane.com/insidious-injury-002/
http://practicalplasticsurgery.org/the-book/
The Pulvertaft Assessment & Management of Acute Hand Injuries (http://www.pulvertafthandcentre.org.uk/courses.asp?pageId=56 )http://journals.lww.com/em-news/Fulltext/2011/12000/ED_Treatment_of_Flexor_Tendon_Injuries.4.aspx
http://bestbets.org/bets/bet.php?id=51
http://www.eatonhand.com/complic/text02.htm http://www.passthefracp.com/Nerves%20of%20the%20Hand.htm
http://bestbets.org/bets/bet.php?id=972
http://bestbets.org/bets/bet.php?id=603
http://bestbets.org/bets/bet.php?id=103
http://bestbets.org/bets/bet.php?id=284
http://bestbets.org/bets/bet.php?id=2205
Documentation
Refer to fingers by name not number.
Use palmar (or volar), dorsal, radial, ulnar (not anterior, posterior, lateral, medial).
Document important positives, as well as important negatives
Examination
Remove rings as soon as possible
X-ray if any likelihood of glass
ElevationThe importance of elevation can not be emphasised enough. The injured hand must always be higher than the heart. Many complications from hand injuries are not from the fracture and associated soft tissue, but from persistent oedema - making healing slower, and surgery more difficult. Elevate!
HealingA fracture in the hand takes 4 weeks to heal clinically, and is faster in children. Radiographic healing can take 4 - 6 months. They begin to heal 7 days after injury. Attempts at closed manipulation after 7 days in children, and adults in 10 days are usually unsuccessful.
Hands should be seen by the specialist less than 5 days after the initial injury.
Tendon InjuriesExtensor Tendon Injuries: Plastics Extensor tendon injuries can be just as devastating as flexor tendon injuries. If suspected, whether partial or full, refer the patient to plastic surgeons. If the injury is less than 50%, conservative management may be considered. A mallet splint should be applied, even if no deformity is apparent.
A mallet finger is loss of extensive extension of the distal interphalangeal joint caused by failure of the terminal slip of the extensor mechanism at its insertion. It is often caused when the extended finger is accidentally stubbed against a hard surface. They should be x-rayed to see whether there is an avulsion fracture present - bony injury is a good prognostic indicator.
Large bony fragment (>1/3 articular surface) = mallet splint + speedy plastics review.
No bony fragment = plastics review clinic 7 - 10 days
Subluxation = speedy plastics review
Flexor Tendon Injuries: PlasticsThere is some controversy about whether to repair these or not. Lacerations can cause flexor tendon injuries, and avulsions from the base of the distal phalynx are commonly missed.
“Rugby shirt finger” is more common in adolescence, and commonly affects the ring finger. Forced extension of the distal phalanx (as in grabbing someone’s collar at rugby) tears the FDP tendon. They can be difficult to diagnose, and a high index of suspicion from the history is needed. They require surgery in <10 days.
Ulnar Collateral Ligament: Plastics The UCL can be ruptured by forced abduction - nowadays from falling when skiing onto the ski-pole. It used to be caused by gamekeeping injuries. The eponymous name “Gamekeeper’s thumb” is being replaced by “Skiiers thumb”. Complete rupture is when the two parts of ligament being separated by the adductor aponeursis (the Stener lesion”).
UCL Sprains: Sometimes the UCL is sprained, and it can be difficult to assess for laxity due to pain. Some texts suggest anaesthetising the UCL and re-assessing. If you are unable to assess the UCL and have a high index of suspicion, treat as per rupture and refer the patient to plastics clinic follow up. If you are unable to assess the UCL and have a low index of suspicion, refer the patient to UCC follow up clinic.
UCL Laxity: If there is laxity >30 degrees, refer the patient to plastics. The thumb should be immobilised in thumb-spica - either tape or plaster of paris.
Avulsion fracture: a UCL sprain or rupture + avulsion fracture should be treated with a scaphoid plaster of paris, and plastics referral.
Nerve InjuriesDigital Nerve Injury: PlasticsThe digital nerve can easily be damaged, and often sensation is intact, but altered. Complaints of altered sensation should be taken seriously.
It is important to have sensation over the edges of the hand - the thumb, the radial aspect of the index finger, or ulnar aspect of the little finger. Repair can be successful up to 2 weeks after injury.
The digital nerves can be repaired up to the level of the DIPJ, although it may be decided not to repair injuries distal to the PIPJ.
When examining the finger for suspected digital nerve damage, it can be useful to test for tactile adherence by running a bic biro along the finger. If there is nerve injury, the biro will slide a lot more easily than normal. It should be a bic biro used as other biros do not have the smooth surface required. Soft Tissue Injuries
Amputations: PlasticsAny amputations, even if there is only a small part amputated should be x-rayed, dressed, bandaged and elevated. Give analgesia, tetanus cover and, broad spectrum antibiotics.
Wrap the amputated part in moist saline swabs and place in a sealed plastic bag surrounded by ice/water mix at 4 degrees.
Amputations should be referred urgently to plastics. If there is problem obtaining haemostasis, and ED seniors can not help, urgent orthopaedic help may be needed.
Finger pad amputations: PlasticsFinger pad amputations are common, especially in children. If skin loss is <1cm2 without bony exposure it may be allowed to heal with non-stick dressings. Larger areas of loss may require grafting. Even if they are small, these wounds need regular follow up and are best followed up in the plastic clinic.
Crush injuries: UCC Review Clinic or GPCrush injuries often cause “burst” injury of fingertip wounds. They should be cleaned, and then closed as appropriate. Remember the wound is likely to swell, so closure can be difficult.
Most of the time these injuries can be reviewed by the GP or Practice Nurse. If you suspect blunt tendon rupture, they need review in plastics clinic. If the area of crush is significant, plastics must be involved.
High pressure injection injuries: PlasticsRefer for immediate exploration and debridement, even if the injury appears minor.
Pulp Infections: GPRemember to X-ray to look for a foreign object or osteomyelitis. Incise over the point of maximal fluctuence, and send the patient home with oral antibiotics (flucloxacillin) and wound care advice.
Pyogenic flexor tenosynovitis: PlasticsKanavel’s signs: tenderness over the flexor tendon, symmetrical swelling of the finger, finger held in flexion, pain on passive extension
Refer for exploration, irrigation, and IV antibiotics.
Phalanx FracturesDistal phalynx fracture (closed): GP/ plasticsAnalgesia and elevation. Buddy strap for symptomatic relief.
These heal well, and do not need orthopaedic or plastic follow up, unless they are complicated. In children, if the fracture is through the growth plate the injury should be followed up by plastics.
Distal phalynx fracture (open): PlasticsThis counts as a complicated fracture and should be referred to plastics for consideration of exploration.
Simple proximal and middle phalangeal fractures: GPThese should be treated with excellent elevation, neighbour strapping and analgesia. Unless requiring manipulation, they do not need follow up. Make sure you have a good lateral to assess the degree of rotation or angulation.
Complicated proximal and middle phalangeal fractures: plasticsAny angulated phalynx fractures should be manipulated - use a needle-holder or pencil placed adjacent to the web space as a fulcrum. You may need to maintain reduction with a volar slap or a Zimmer splint.
Refer speedily for surgical fixation if reduction is unsatisfactory or can not be maintained.
Phalangeal Dislocations: plasticsAlways X-ray before reduction and then reduce under digital nerve block or entonox with traction and gentle manipulation. Check integrity of the collateral ligaments after reduction. Buddy strap, elevate, analgesia and provide follow up. Metacarpal fractures
The management of a metacarpal fracture depends on which bit of the metacarpal, which finger, and how angulated it is. Elevation is the most important component of treatment!
Metacarpal Head: PlasticsApply a volar slab, encourage elevation, and refer to plastics.
Metacarpal Neck and Shaft: plasticsCarefully assess degree of rotation and then apply a volar slab or ulnar gutter. Encourage elevation. Most fractures are treated non-operatively, especially in the middle and index metacarpal.
Refer acutely for operative intervention if any rotational deformity, more than 5mm shortening or more than 10o, 10o, 20o, 20o of angulation respectively for 2nd - 5th metacarpals.
Metacarpal Base: plasticsCheck lateral x-ray carefully to ensure the carpo-metacarpal joint is not dislocated, as metacarpal base fractures are frequently fracture-dislocations. These are typically unstable and should be treated with a volar slab or ulnar gutter, elevated, and referred to plastics.
Thumb Base fractures: plasticsIntrarticular: Bennett’s (fracture fragment on ulnar side of thumb)
Rolando (fracture fragment on radial side of thumb)
Apply a bennett’s POP (like a scaphoid but thumb abducted) and refer to plastics for speedy operative repair.
Extraarticular: Check dorsal angulation. If angulated more than 30o or shortened more than 4mm, need speedy operative repair. If non-angulated, refer to plastics for follow up.
Thumb dislocations: plasticsReduce thumb dislocations, then immobilise in a scaphoid POP + follow up.
.
Little (5th) MC dislocation: plasticsMay be associated with fracture - refer after reduction for internal fixation.
MCPJ Dislocation: plasticsAfter reduction assess integrity of collateral ligaments. Then immobilise in 15 degree flexion. If failed reduction, refer for open reduction
Other Hand ProblemsVolar plate injury: plasticsHyperextension at the PIPJ injures the volar plate at the base of the middle phalanx without evidence of bony involvement. Examination shows fusiform swelling of the PIPJ with tenderness over the volar aspect. Treat with buddy strapping to adjacent fingers. Plastics review needed to ensure full mobility regained.
Locked Finger: plasticsThis is common in elderly patients with osteoarthritis. There is often no history of trauma. Refer for hand surgeon opinion - do not try to straighten the affected finger.
Trigger finger/ thumb: GPSpecialist to inject steroid injection into the flexor tendon sheath. GP to refer to orthopaedics.
Fight Bite: PlasticsSuspect a fight bite in any patient presenting with wounds on the dorsum of the hand over the index, middle, ring or little finger MC heads of having sustained a human bite, what ever history is given. Many plastic surgery centres will thoroughly irrigate all of these wounds in theatre, so discuss them all.
Reading and References
http://academiclifeinem.com/pv-card-metacarpal-fractures/
http://learning.bmj.com/learning/module-intro/managing-minor-skiing-snowboarding-injuries-primary-care.html?moduleId=5003325&searchTerm=%E2%80%9Chand%E2%80%9D&page=3&locale=en_GB
https://gmep.org/media/13991
http://lifeinthefastlane.com/insidious-injury-002/
http://practicalplasticsurgery.org/the-book/
The Pulvertaft Assessment & Management of Acute Hand Injuries (http://www.pulvertafthandcentre.org.uk/courses.asp?pageId=56 )http://journals.lww.com/em-news/Fulltext/2011/12000/ED_Treatment_of_Flexor_Tendon_Injuries.4.aspx
http://bestbets.org/bets/bet.php?id=51
http://www.eatonhand.com/complic/text02.htm http://www.passthefracp.com/Nerves%20of%20the%20Hand.htm
http://bestbets.org/bets/bet.php?id=972
http://bestbets.org/bets/bet.php?id=603
http://bestbets.org/bets/bet.php?id=103
http://bestbets.org/bets/bet.php?id=284
http://bestbets.org/bets/bet.php?id=2205
Nail Injuries
After looking at the available resources, this is my summary of the suggested management for nail injuries in MY hospital. Please do comment with what you'd do in your hospital.
Subungal haematoma: GP follow up
There is no evidence that trephining a subungal haematoma reduces pain, or alters outcome. Some sources suggest draining if it is >50% of the nail.
If the patient has a lot of pain from their haematoma, trephining is recommended.
Twisting a green needle over an area of haematoma normally allows blood to escape. A red hot paperclip is no longer recommended. This procedure is normally well tolerated, and a digital nerve block is rarely needed.
Removing the nail to look for nail bed lacerations is low yield, and no longer routinely recommended.
There is no evidence that antibiotics are helpful, even if there is an associated fracture.
No follow up is needed for the subungal haematoma itself - fractures may need further management.
Nailbed lacerations: GP follow up
If the nail has been ripped off and is in-tact, consider replacing the nail to protect the nail bed.
Foreign Body under the nail: GP follow up
Perform a digital nerve block and remove the foreign body with fine forceps.
If you need to cut away the nail, take as smaller wedge out as possible.
Paronychia: GP follow up
References
http://bestbets.org/bets/bet.php?id=972
http://bestbets.org/bets/bet.php?id=603
http://bestbets.org/bets/bet.php?id=103
http://bestbets.org/bets/bet.php?id=284
http://bestbets.org/bets/bet.php?id=2205
Subungal haematoma: GP follow up
There is no evidence that trephining a subungal haematoma reduces pain, or alters outcome. Some sources suggest draining if it is >50% of the nail.
If the patient has a lot of pain from their haematoma, trephining is recommended.
Twisting a green needle over an area of haematoma normally allows blood to escape. A red hot paperclip is no longer recommended. This procedure is normally well tolerated, and a digital nerve block is rarely needed.
Removing the nail to look for nail bed lacerations is low yield, and no longer routinely recommended.
There is no evidence that antibiotics are helpful, even if there is an associated fracture.
No follow up is needed for the subungal haematoma itself - fractures may need further management.
Nailbed lacerations: GP follow up
If the nail has been ripped off and is in-tact, consider replacing the nail to protect the nail bed.
Foreign Body under the nail: GP follow up
Perform a digital nerve block and remove the foreign body with fine forceps.
If you need to cut away the nail, take as smaller wedge out as possible.
Paronychia: GP follow up
References
http://bestbets.org/bets/bet.php?id=972
http://bestbets.org/bets/bet.php?id=603
http://bestbets.org/bets/bet.php?id=103
http://bestbets.org/bets/bet.php?id=284
http://bestbets.org/bets/bet.php?id=2205
Sunday, 23 February 2014
Paronychia
I've put all my musculoskeletal notes into this blog - as otherwise the other one is going to get pretty full. It's only one core presentation, but musculoskeletal covers a lot!
Paronychias
http://lifeinthefastlane.com/minor-injuries-007/
http://journals.lww.com/em-news/Fulltext/2010/11000/InFocus__Fingertip_Problems__Acute_Paronychia.5.aspx
http://journals.lww.com/em-news/Fulltext/2003/09000/The_Clinical_Approach_to_Paronychia.15.aspx
http://academiclifeinem.com/trick-of-the-trade-toe-paronychia-splinting/
http://journals.lww.com/em-news/blog/theproceduralpause/pages/post.aspx?PostID=3
Inflammatory involvement of the fold of the nail on the radial or ulnar side.
 |
| Picture from lifeinthefastlane.com who borrowed it from www.aafp.org |
The most common cause is trauma to the cuticle or nail fold, innoculating staph aureus. Cases can be related to antiretroviral therapy, and from sucking fingers. Strep pyrogenes, pseudomonas pyocyanea and proteus vulgaris have also been seen.Rapid onset of symptoms.
Management
Make a longitudinal incision parallel to the nail edge. You should be able to separate the cuticle from the underlying nail, exposing the potential space that is filled with pus. The skin is not actually incised - a bonus for any diabetics.
Hot soaks may improve things in just 20minutes.
Home with advice to soak in saline and wash regularly +elevation. Should be asymptomatic in 3- 5 days!
Give antibiotics if tracking cellulitis
Chronic Paronychia
This is a multifactorial inflammatory reaction of the proximal nail fold to irritants and allergens or repeated paronychial infections.
Herpetic Whitlow - don't cut it!
http://pedemmorsels.com/herpetic-whitlow-dont-cut-it/
http://drhem.com/tag/herpetic-whitlow/
These happen commonly in children, adolescents/adults (may be associated with genital HSV) and adults (medical professionals who get inoculated by patients).
It starts with pain + tingling, then swelling and redness, constitutional symptoms. Then you get 1 or more vesicles that enlarge. Remain for 7 - 10 days, then crust over. Peeling occurs in a week.
Treatment: check other mucous membranes for vesicles, don't incise, pain management, dry dressings, needle aspiration of larger tense vesicles, aciclovir - controversial evidence.

Be careful your paronychia or whitlow it isn't a mimic:
• Squamous cell carcinoma
• Malignant melanoma
• Malignant tumors
• Eczema or psoriasis
• Reiter’s syndrome
Subscribe to:
Posts (Atom)










